The Connection Between Diabetes and Obesity: Managing Your Weight for a Healthier Future
Diabetes and obesity are two health issues that often go hand in hand. In this article, we will discuss the strong link between diabetes and obesity, and explore effective strategies for managing weight in the context of diabetes. Understanding this connection and taking positive steps toward weight management can lead to a healthier and happier life.
Understanding Diabetes and Obesity
Diabetes is a medical condition that affects how your body uses glucose, or sugar. Our bodies need glucose for energy, and insulin, a hormone produced by the pancreas, helps regulate the amount of glucose in our blood. There are two main types of diabetes:
- Type 1 Diabetes: In this type, the immune system mistakenly attacks and destroys insulin-producing cells in the pancreas. People with Type 1 diabetes must take insulin injections or use an insulin pump to manage their blood sugar levels.
- Type 2 Diabetes: This is the most common type of diabetes and is often associated with lifestyle factors, including diet and physical activity. In Type 2 diabetes, the body doesn’t use insulin properly, leading to high blood sugar levels.
Obesity is a condition characterized by an excessive amount of body fat. It’s usually measured using the Body Mass Index (BMI), which takes into account your height and weight. A BMI of 30 or higher is considered obese. Obesity can increase the risk of various health problems, including heart disease, stroke, and, as we’ll discuss in detail, diabetes.
The Connection Between Diabetes and Obesity
Obesity is a well-established risk factor for Type 2 diabetes. When you carry excess body fat, especially around the waistline, it can affect how your body uses insulin. This is known as insulin resistance. As your body becomes more resistant to insulin, blood sugar levels rise, increasing the risk of developing Type 2 diabetes.
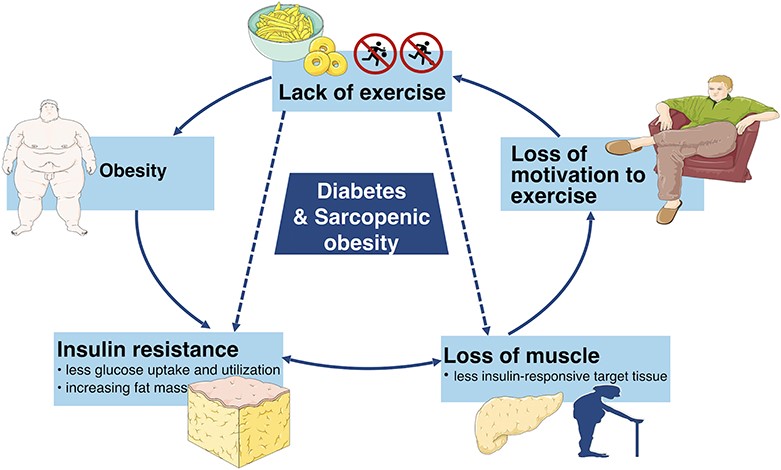
The Vicious Cycle
The link between diabetes and obesity creates a vicious cycle. Obesity increases the risk of diabetes, and having diabetes can make it harder to lose weight. High blood sugar levels can lead to increased hunger and cravings for sugary and high-calorie foods, making it challenging to maintain a healthy weight.
How Does Obesity Cause Diabetes?
Obesity can cause diabetes through various mechanisms:
- Insulin Resistance: Excess body fat, particularly in the abdominal area, is associated with increased insulin resistance. When fat cells become enlarged due to obesity, they release substances that interfere with insulin’s ability to control blood sugar levels. This resistance means that more insulin is needed to keep blood sugar in check, putting extra strain on the pancreas.
- Inflammation: Obesity triggers chronic low-grade inflammation throughout the body. This inflammation contributes to insulin resistance and can further impair the body’s ability to use glucose efficiently.
- Fat Deposition in the Liver: In obese individuals, fat can accumulate in the liver, a condition known as non-alcoholic fatty liver disease (NAFLD). NAFLD is associated with insulin resistance and an increased risk of Type 2 diabetes.
- Hormonal Changes: Obesity can disrupt the balance of hormones involved in glucose regulation, such as adiponectin and leptin. These hormonal changes can further contribute to insulin resistance and the development of diabetes.
- Beta Cell Dysfunction: The pancreas contains cells called beta cells that produce insulin. In obesity, the increased demand for insulin can lead to beta cell dysfunction and reduced insulin production. This decline in insulin secretion exacerbates high blood sugar levels.
Strategies for Weight Management in Diabetes
Now that we understand the link between diabetes and obesity, let’s explore some strategies for managing weight when you have diabetes.
- Healthy Eating Habits
• Balanced Diet: Focus on a balanced diet that includes a variety of foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats.
• Portion Control: Be mindful of portion sizes. Using smaller plates can help with portion control.
• Limit Sugary Foods and Drinks: Reduce or eliminate sugary snacks, sugary drinks, and desserts from your diet. Opt for sugar-free or low-sugar alternatives.
• Fiber-Rich Foods: Include fiber-rich foods like whole grains, legumes, and vegetables in your meals. Fiber can help you feel full and satisfied.
• Regular Meals: Try to eat regular meals and snacks throughout the day to prevent overeating later. - Physical Activity
• Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise per week. Activities like brisk walking, swimming, or cycling can help you burn calories and improve insulin sensitivity.
• Strength Training: Incorporate strength training exercises into your routine to build muscle, which can boost your metabolism.
• Stay Active: Look for opportunities to be active throughout the day, such as taking the stairs instead of the elevator or going for short walks.
• Consult a Healthcare Provider: Before starting a new exercise program, especially if you have diabetes complications, consult your healthcare provider for guidance. - Mindful Eating
• Listen to Your Body: Pay attention to your body’s hunger and fullness cues. Eat when you’re hungry and stop when you’re satisfied.
• Avoid Emotional Eating: Be mindful of eating in response to emotions rather than hunger. Find alternative ways to cope with stress or emotional triggers.
• Slow Down: Eat slowly and savor each bite. This can help you enjoy your food more and prevent overeating. - Monitoring Blood Sugar Levels
• Regular Testing: Monitor your blood sugar levels as recommended by your healthcare provider. Understanding how different foods and activities affect your blood sugar can help you make better choices.
• Medication Adjustments: Work closely with your healthcare team to adjust diabetes medications or insulin if necessary, based on your blood sugar levels and weight management goals. - Support and Education
• Diabetes Education: Consider attending diabetes education classes or programs. These can provide valuable information on nutrition, exercise, and diabetes management.
• Support Groups: Joining a support group or connecting with others who have diabetes can offer emotional support and practical tips for weight management. - Consulting Healthcare Professionals
• Registered Dietitian: Consult a registered dietitian who specializes in diabetes care. They can help you create a personalized meal plan and provide guidance on portion control.
• Endocrinologist: If you have complex diabetes management needs, consider seeing an endocrinologist, a doctor who specializes in hormone-related conditions like diabetes. - Setting Realistic Goals
• Achievable Goals: Set achievable weight loss goals. Small, gradual changes are more sustainable and can lead to long-term success.
• Patience: Understand that weight management takes time. Be patient with yourself and stay committed to your health. - Medication and Surgery
• Prescription Medications: In some cases, healthcare providers may prescribe medications that can aid in weight management. These should be used under medical supervision.
• Bariatric Surgery: Bariatric surgery may be considered for individuals with severe obesity and diabetes that is difficult to manage through other means. It is a significant step and should be discussed with healthcare professionals.
Conclusion
The link between diabetes and obesity is undeniable, but it’s important to remember that you can take control of your health. By understanding this connection and implementing effective weight management strategies, you can reduce the risk of diabetes complications and lead a healthier, more fulfilling life. Remember, small changes can lead to big improvements, so take it one step at a time on your journey to better health.
References:
- DiabetesOrg. (n.d.). Weight Loss And Diabetes. Retrieved from https://www.diabetes.org.uk/guide-to-diabetes/enjoy-food/eating-with-diabetes/whats-your-healthy-weight/lose-weight
- Kelly. (n.d.). Does Obesity Cause Diabetes? Retrieved from https://www.healthline.com/health/diabetes/does-obesity-cause-diabetes
- Nuha. (n.d.). Obesity And Weight Management For The Prevention And Treatment Of Type 2 Diabetes: Standards Of Care In Diabetes—2023. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9810466/#:~:text=In%20people%20with%20type%202,11%2C19%E2%80%9323).
- Wilding. (n.d.). The Importance Of Weight Management In Type 2 Diabetes Mellitus. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4238418/

